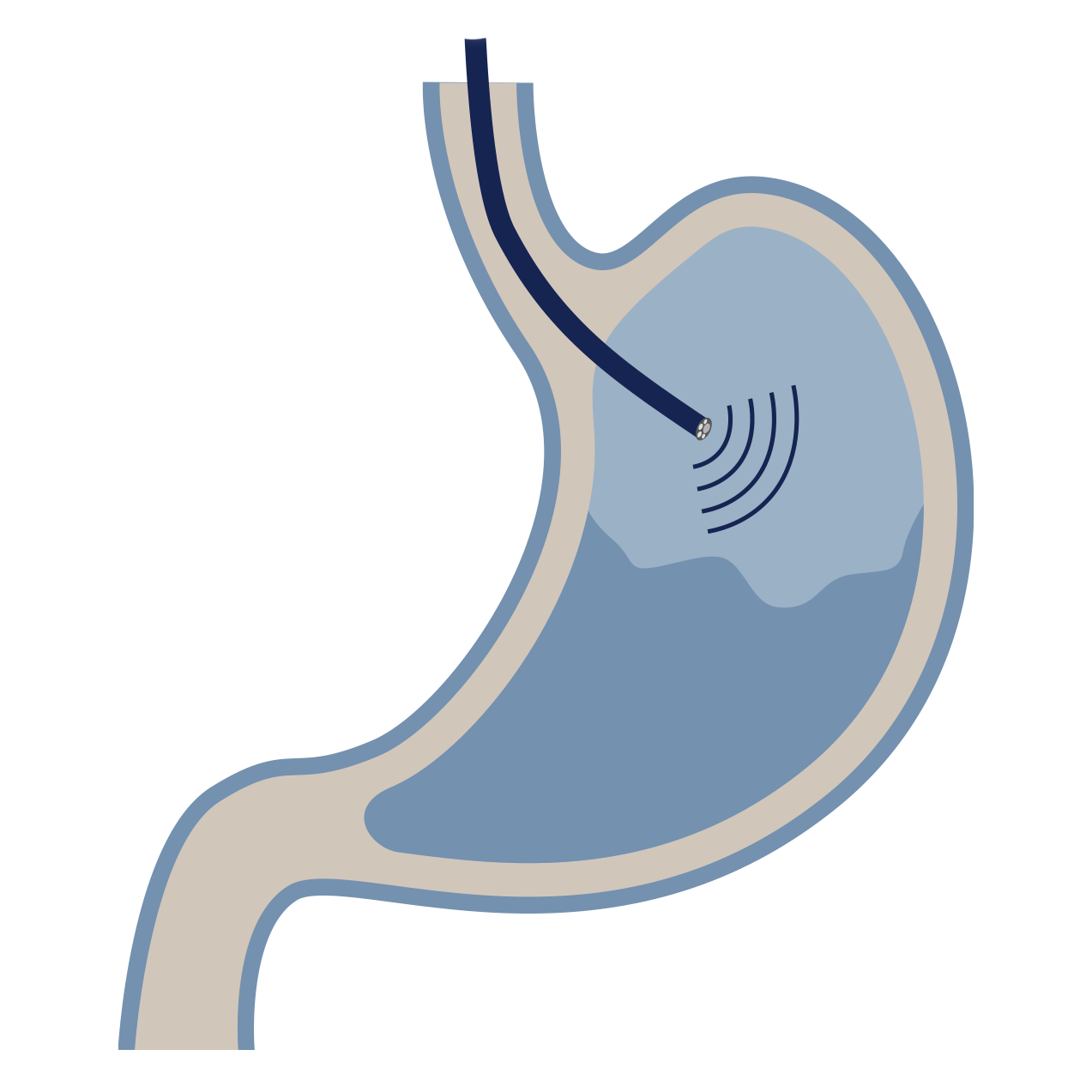
Endoscopic Ultrasound (EUS)
What is an endoscopic ultrasound (EUS)?
Endoscopic ultrasound (EUS) is an advanced, minimally invasive procedure that uses a special endoscope equipped with an ultrasound probe at its tip. This allows Dr Selvanderan to generate detailed, high-frequency ultrasound images of the internal organs adjacent to the digestive tract, such as the pancreas, bile ducts, liver, and lymph nodes. EUS provides detailed imaging superior to external ultrasound and is integral for staging certain cancers or sampling abnormal growths.
Why might you need an EUS?
EUS is mainly a diagnostic and staging tool for conditions in the upper GI tract, chest, and adjacent organs such as the gallbladder, pancreas and bile ducts. Reasons for performing an EUS include:
Pancreas assessment: Diagnosing and staging pancreatic masses (including cancer), chronic pancreatitis, and cysts.
Bile duct assessment: Evaluating strictures, stones (especially small stones not seen on other scans), and assessing the depth of invasion of bile duct tumours.
Staging cancers: Determining the depth of invasion of oesophageal, stomach, or rectal cancers, and assessing local lymph nodes before surgery.
Submucosal lesions: Investigating abnormal growths beneath the lining or in the wall of the digestive tract.
Fine-needle aspiration (FNA) or biopsy (FNB): Passing a needle through the endoscope, guided by the ultrasound image, to safely obtain tissue samples from masses or lymph nodes.
Preparing for your EUS
Fasting: For an endoscopic ultrasound of the upper GI tract, you must not eat or drink anything (including water) for a specified period, typically 6 hours prior to the procedure.
Medication: You will be advised about which medications to stop or adjust, particularly blood-thinners, if a biopsy (FNA/FNB) is planned.
What to expect?
EUS is performed by Dr Selvanderan in the endoscopy suite. The procedure typically takes 30-60 minutes, depending on whether a biopsy is required.
Sedation: Dr Selvanderan works with a specialist anaesthetist for the procedure. Most patients receive light intravenous sedation (a 'twilight sleep') to ensure comfort and minimal memory of the procedure. A local anaesthetic spray may also be applied to the back of your throat.
During the procedure: You will lie on your left side. The echo-endoscope is passed through the mouth, into the oesophagus, stomach, and duodenum. The ultrasound probe is positioned against the wall of the GI tract to visualise the adjacent structures. If an FNA/biopsy is needed, a fine needle is passed through the scope and into the target lesion.
Your Recovery
Due to the deep sedation or anaesthetic, you will be monitored in a recovery area.
Discharge: You will usually be ready to go home within 1-2 hours after the procedure.
Post-sedation: You must not drive or operate machinery for the rest of the day. You must have a responsible adult escort you home and stay with you.
Sore throat: It is common to have a mild sore throat, hoarseness, or bloated feeling, which usually resolves within 24 hours.
Results: Dr Selvanderan will discuss the preliminary findings with you before you leave. A procedure report will be sent to your referring doctor. Biopsy results typically take several days and will be communicated to you and your referring doctor subsequently. Where required, a follow-up consultation will be arranged by Dr Selvanderan’s rooms.
Risks
EUS is a safe procedure, but risks are slightly higher if a fine-needle aspiration (FNA) or fine-needle biopsy (FNB) is performed. Potential risks include:
Bleeding: Minimal if no biopsy is performed. If biopsy is performed, a small risk of minor bleeding exists
Infection: Rare, but can occur, especially when draining cysts. Antibiotics may be given preventatively.
Pancreatitis: A very small risk, primarily when sampling lesions close to the pancreatic duct.
Perforation: Extremely rare.
Expert investigation with endoscopic ultrasound
Dr Shane Selvanderan provides expert diagnostic and therapeutic endoscopic ultrasound (EUS), offering highly detailed imaging and safe tissue acquisition (FNA/biopsy) for the diagnosis and staging of various gastrointestinal and pancreaticobiliary conditions.