Endoscopic Submucosal Dissection (ESD)
What is an endoscopic submucosal dissection (ESD)?
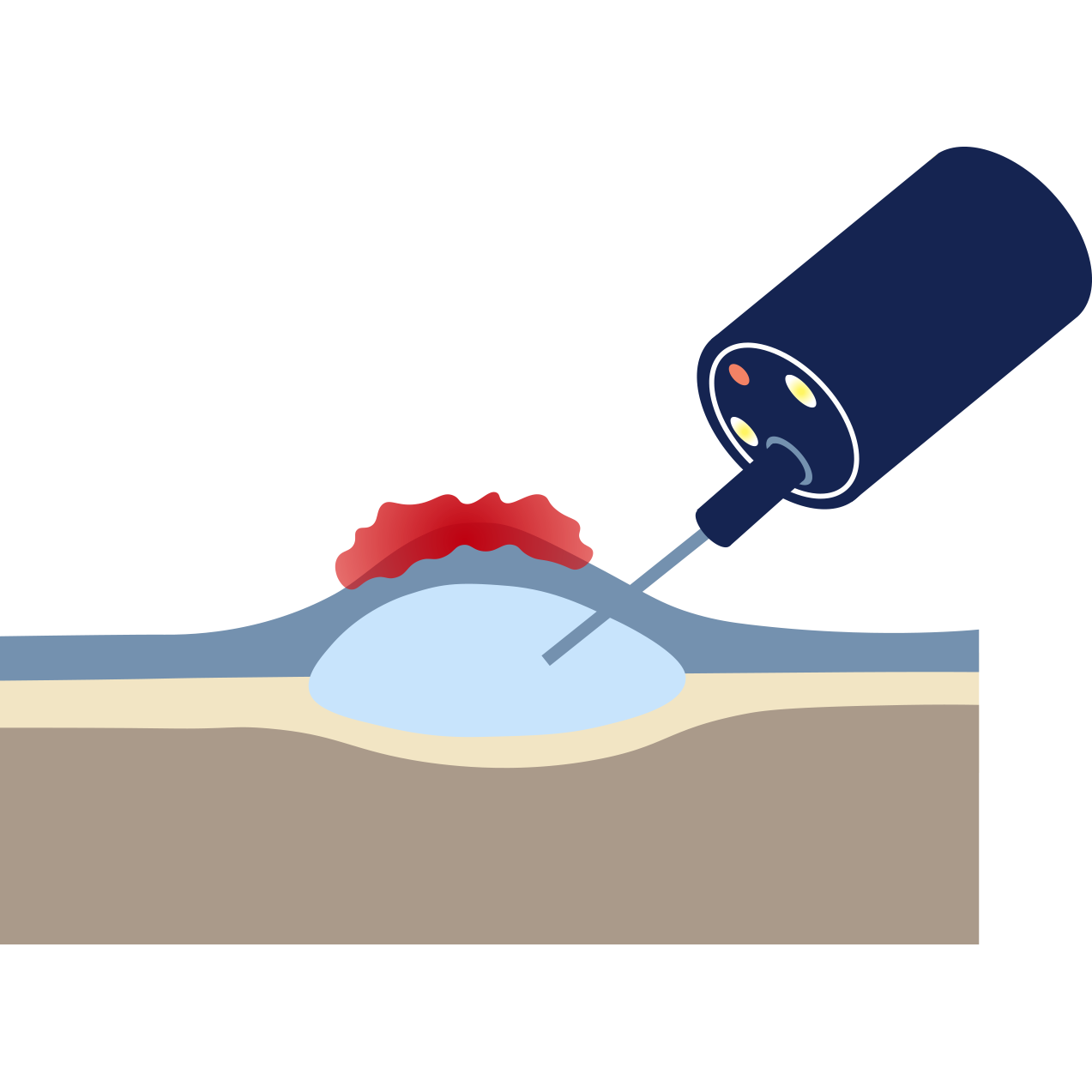
Endoscopic submucosal dissection (ESD) is an advanced, highly technical endoscopic procedure used to remove much larger or deeply invasive superficial cancers or polyps in a single, intact piece (en bloc resection). It is a more complex and technically demanding procedure than EMR.
Using specialised knives only 1 - 2 mm in length passed through the endoscope, Dr Selvanderan carefully dissects the lesion away from the underlying muscle layer, entirely removing the lesion in one piece. This single-piece removal is vital for accurate pathology staging.
Why might you need an ESD?
ESD is reserved for lesions that are large, have a high suspicion of early cancer, and where an en bloc resection is crucial for accurate staging and cure. Reasons for ESD include:
Large lesions: Removal of very large, flat polyps or early cancers in the oesophagus, stomach, or colon that are unsuitable for piecemeal EMR.
High-risk early cancer: Resection of early cancers where accurate, single-piece removal is required to confirm the depth of invasion and ensure a curative margin.
Recurrent lesions: Removing lesions that have recurred after previous polypectomy or EMR.
Preparing for your ESD
Fasting: Standard fasting instructions (typically 6 hours).
Bowel preparation (for colon or rectum ESD): Full, excellent bowel preparation is essential to ensure a clear view.
Medication: All blood-thinning medications generally need to be stopped otherwise the bleeding risk is significant. Specific instructions will be provided.
What to expect?
ESD is a complex, lengthy, and meticulous procedure performed by Dr Selvanderan, usually under general anaesthesia, and can take anywhere from 1-3 hours.
Anaesthesia: General anaesthesia is often required for patient comfort and to ensure the precision needed for the dissection.
During the procedure: The lesion is marked, and fluid is injected beneath it. Specialised knives are used to cut around the perimeter of the lesion and then dissect the lesion entirely away from the deeper muscle layer. Once the lesion is removed, the wound may be closed with endoscopic clips.
Your Recovery
ESD involves a slightly increased risk profile and requires close observation.
Hospital stay: Patients may require an overnight stay for observation.
Diet: A modified diet for a few days following the procedure may be advised to allow the large resection site to heal.
Results: Dr Selvanderan will discuss the preliminary findings with you before you leave. A procedure report will be sent to your referring doctor. Pathology from the removed tissue typically take several days to be reported and will be communicated to you and your referring doctor subsequently. Where required, a follow-up consultation will be arranged by Dr Selvanderan’s rooms.
Risks
ESD is an advanced procedure with higher risks than routine endoscopy or EMR. Dr Selvanderan will discuss these risks with you in detail at a consultation prior to the procedure.
Perforation: The most significant risk, as the dissection is performed close to the muscle layer
Delayed bleeding: The risk is similar to or slightly higher than EMR, sometimes requiring further endoscopic management.
Stricture: The resection of very large lesions, especially in the oesophagus, can lead to subsequent narrowing (stricture formation), which may require future endoscopic dilation.
Expert treatment and answers
Dr Shane Selvanderan is one of a few Melbourne gastroenterologists with international training and expertise in endoscopic submucosal dissection (ESD). He utilises this curative technique to remove large, complex gastrointestinal lesions and early cancers in a single piece, maximising the chances of cure while avoiding major surgical resection.